If you’re wondering whether nerve monitoring will be utilized during a thyroid or parathyroid operation at the Advanced Thyroid and Parathyroid Center, the answer is no.
There has been much controversy over the use of intraoperative nerve monitoring during thyroid and parathyroid surgery. The concept is quite simple. Nerve monitoring uses a special endotracheal tube with electrodes which detect movement of the vocal cords against them. The wires from the electrodes are then plugged into a machine that makes an audible beeping sound when the nerve is being agitated during the operation. When a surgeon is dissecting tissue around the recurrent laryngeal nerve (nerve that makes the vocal cords move), the beeping sound serves as a signal to be careful and not injure or cut the nerve. Seems quite simple and useful, but nobody has been able to prove that it is beneficial in terms of decreasing the risk of adverse effects of temporary or permanent injury to the recurrent laryngeal nerve.
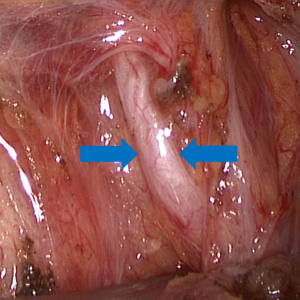
The gold standard for protecting the recurrent laryngeal nerve is visual identification during surgery using the surgeon’s eyes.
After much experience with nerve monitoring, its use in our practice has been abandoned for the following reasons.
-The nerve monitor doesn’t always work appropriately. A single grounding electrode wire slipping out of the skin or the endotracheal tube moving causes the monitor to malfunction.
-The nerve may not stimulate during the operation, but may work normally after the operation.
-The nerve may stimulate during the operation, but may be weak after the operation.
-The technology simply is not reliable enough to warrant any change in the surgeon’s technique or procedure based on the information it provides.
No surgeon is perfect, but the surgeon’s eye is the most sensitive means of finding and protecting the nerve during surgery. These difficulties inherent to the technology are why it has not been proven to decrease the rates of nerve injury. The only thing nerve monitoring has been proven to do is increase the cost of the operation by several hundred dollars because of the disposable tube and nerve stimulator. Has your health insurance premium decreased recently?
One might wonder why nerve monitoring is used at all. Many surgeons who use the technology work in teaching institutions. They feel it has value in teaching resident physicians, and they write papers about its use. It’s not wrong to use nerve monitoring, but it’s really analogous to using the navigation system on your car or smartphone to drive home from work. Maybe it’s helpful the first time or two, but after you’ve done it many times, it’s unnecessary.
